The physiology behind cardiac dysrhythmias and electrocardiography in diagnostics is fascinating. I worked part-time as a telemetry and ECG technician at Abrazo Heart Hospital while in graduate school at Arizona State University, where I was studying under a cardiovascular exercise physiologist. The great thing about each 12-hour shift is that it was different. Because the hospital specializes in heart and vascular treatments, each day would bring its own challenges. As patient statuses change or someone arrives through the ER, they have surgery or a procedure, anything can be expected. To be successful, it is necessary to consistently research information to improve proficiency – in journals, textbooks and self-study websites, discuss information with peers and nurses to expand all efforts to do a great job, and in turn, pass along new knowledge to help the staff.
The experience prompted me to start compiling an ECG Knowledge Bank – a list of websites deemed worthwhile for all of those hard working folks in healthcare, academia, cardiac rehabilitation, firefighting – anyone that needs to obtain or maintain a thorough and accurate understanding of rhythm diagnostics. There is also discussion section on tricky rhythms and ways to differentiate them, as clinical reality is quite different from a textbook. This is a long term work in progress – there will be updates, so save the link if you find it useful, and please contact me if there is something you’d like to see added or expanded upon. Cheers!
ECG References:
- LITFL ECG Library: Life In The Fast Lane (LITFL) “is a medical blog and website dedicated to providing free online emergency medicine and critical care insights and education for everyone, everywhere…anytime.” Authors of the site content are emergency physicians and intensivists based in Australia and New Zealand. Very, very thorough explanation of a vast amount of rhythms – I use this site often as it seems to cover everything.
- SkillStat ECG Simulator: Awesome for practice. The free simulator provides a continuously running 6 second strip of the 27 most common cardiac rhythms, and has a setting for both practice and a quiz.
- ECGpedia: This site consists of a free, complete ECG tutorial and textbook to which anyone can contribute. It is helpful for quick reference and easy to navigate, and I have found it contains quality information on an array of populations, such as athletes, children and different ethnicities. There is also some interesting background on the history of ECG technology.
- Ventricular Arrhythmias in the Absence of Structural Heart Disease. This is a wonderful article written by Dr. Eric Prystowsky, et al., published in 2012 by the Journal of the American College of Cardiology. Very thorough, with lots of discussion on the pathophysiology, and many ECG figures. Table 1 is very helpful in outlining the arrhythmias discussed within the article.
When you just can’t put your finger on it… we attempt to. (click each topic to jump to it)
- Is it coarse atrial fibrillation, atypical atrial flutter, or multifocal atrial tachy?
- Tachycardia: What subtype is it reeeeeally?
- Dysrhythmia or arrhythmia?
- Pacemakers: When they don’t work
- Can junctional rhythms have a positive P wave in lead II?
- Measuring the QT Interval
Is it coarse atrial fibrillation, atypical atrial flutter, or multifocal atrial tachy?
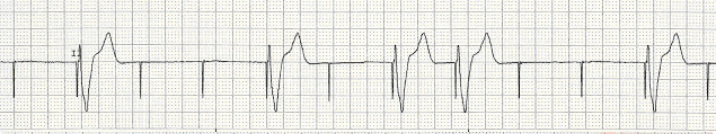
A few times I have found myself thinking this very question. Of course, it is very important to get it right because the underlying cause of each is completely different. We know atrial flutter has a distinct sawtooth F (fibrillation) wave morphology, but so does coarse A Fib (F waves are >0.5 mm). In addition, sometimes atrial flutter can have an irregular heart rhythm (called atypical atrial flutter), where R-R intervals are not equal, and there is a varying number of F waves between each QRS. So it can be easy to confuse the two. Multifocal atrial tachycardia (MAT) is also typically irregularly irregular, with at least three different P wave morphologies and PR intervals. To figure it out:
- A Fib will have varying F wave morphologies (i.e. different amplitudes/spacing). The atrial rate is typically 400-600 bpm.
- A Flutter will have more consistent F waves, even if the ventricular rhythm is irregular. The atrial rate is typically 200-400 bpm, lower than A Fib.
- MAT will have defined P waves and PR intervals.

Tachycardia: What subtype is it reeeeeally?
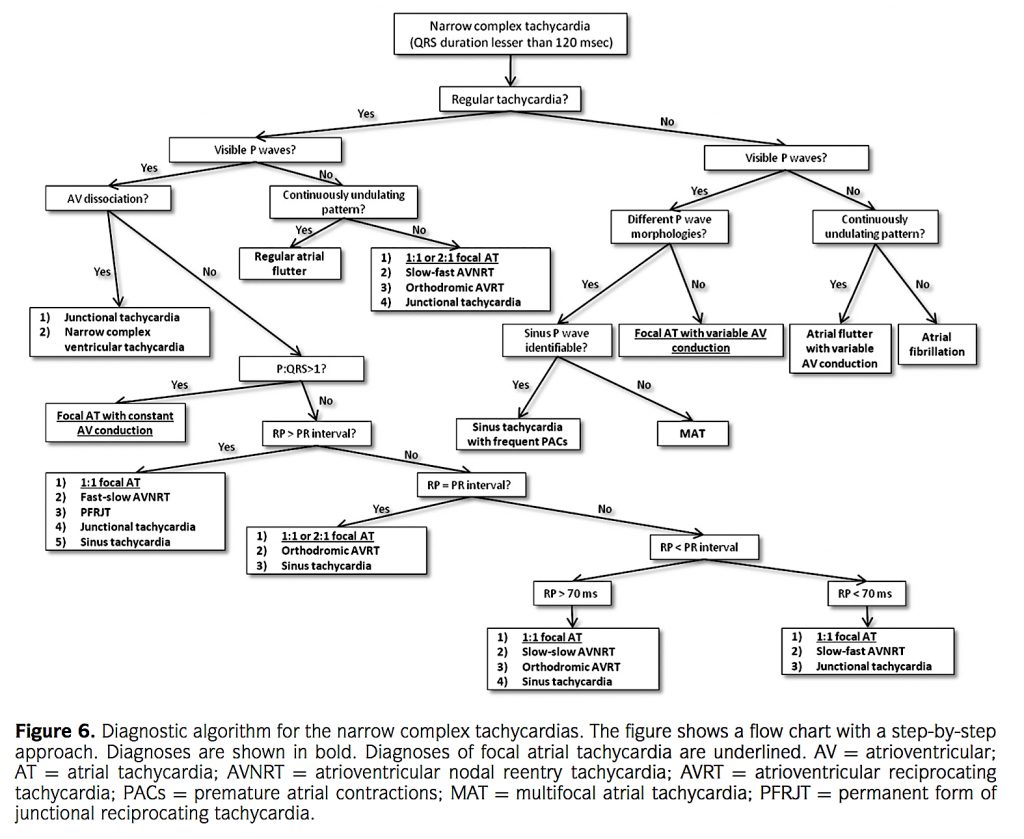
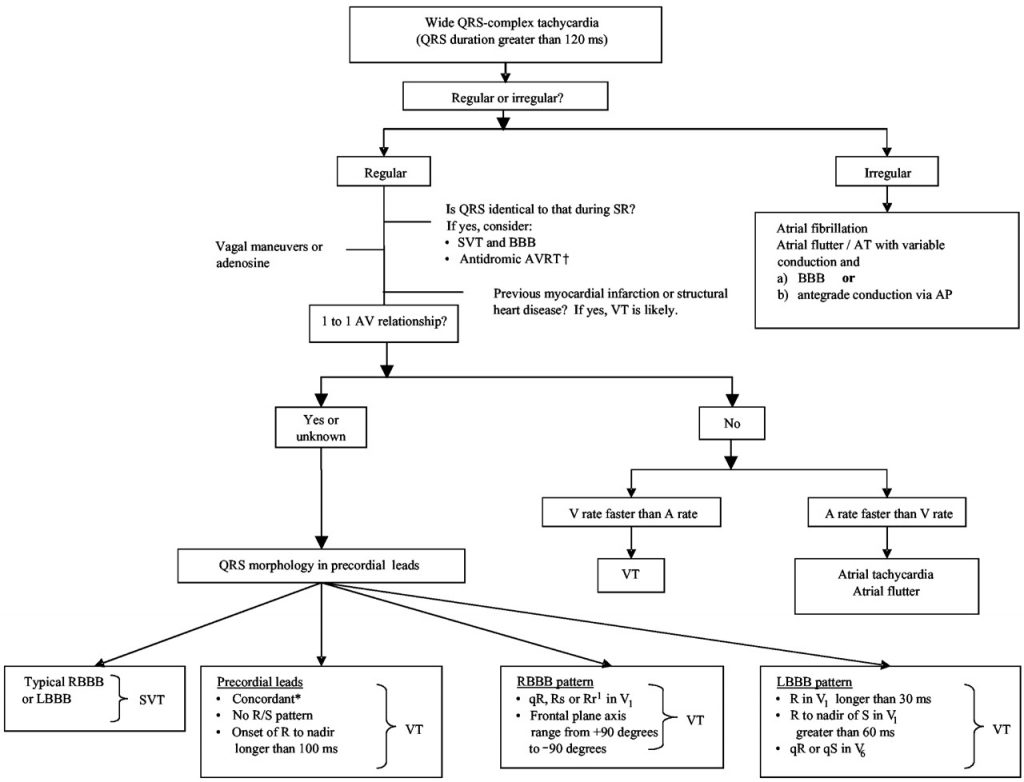
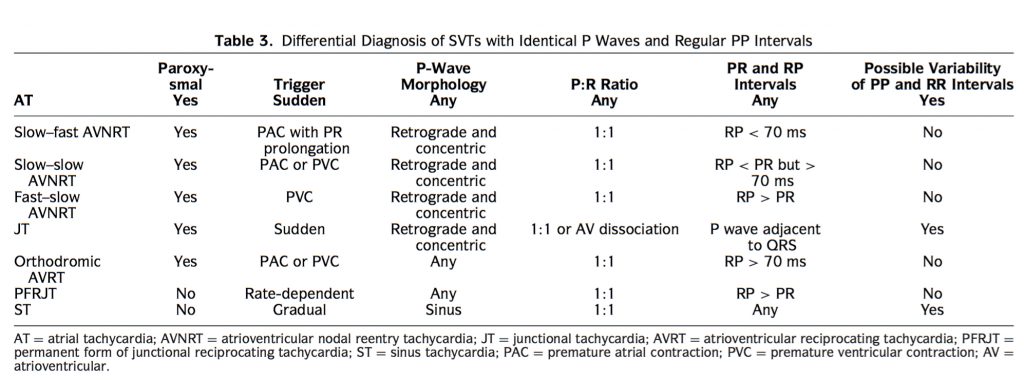
There are three major classifications of tachycardia (heart rate >100 bpm), named after the origin: sinus, atrial/supraventricular, and ventricular. It is common to label many fast atrial rates as supraventricular tachycardia (SVT). Same with ventricular tachycardia (VT); it is used as a “catch all” name quite often. But, some of the subtle differences are extremely important to note, and the necessity for proper identification should not come as a surprise. Here is a quick down and dirty outline, with explanations for patients without a pre-existing bundle branch block (where a wide QRS of >120 ms would be present). There are also two algorithms at the end: one for narrow complex tachycardias, and another for wide complex tachycardias. Click on them to open in a new window.
- Sinus tachycardia (ST). Just a fast version of normal sinus rhythm. Steadily sustained. It doesn’t come on suddenly, and is very rarely associated with a serious underlying condition.
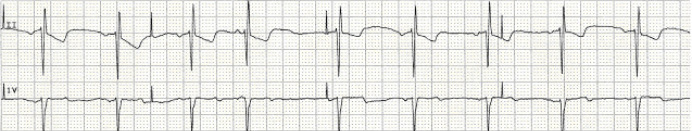
- Atrial/supraventricular tachycardias. According to an article published in the British Medical Journal (BMJ), “Any tachyarrhythmia arising from the atria or the atrioventricular junction is a supraventricular tachycardia.” These narrow-complex tachycardias are difficult to discern. In this case, several things need to be considered. First, and simply, you need to consider the length the patient is experiencing the rate/rhythm. If it is short and comes on abruptly, its noted as paroxysmal (as in PSVT or PAT). Also, see the atrial tachycardia algorithm at the end of this section, as it is very helpful.
- Supraventricular tachycardia (SVT or PSVT). This term is often used as a “catch all” for most ectopic tachy rhythms originating in the atrium, however, it does have it’s own distinctions. PSVT typically starts and stops abruptly and is >135 bpm. QRS is typically narrow.
- AV Nodal Reentrant Tachycardia (AVNRT). Accounts for roughly half of all PSVTs. This is technically a junctional tachycardia.
- AV Reciprocating Tachycardia. Also a junctional tachycardia.
- Sino-Atrial Reentrant Tachycardia. Very rare; mimicks ST but starts and stops abruptly.
- Atrial tachycardia (AT or PAT). Do not get this confused with A Fib. Here, the rhythm is regular (A Fib is irregular). AT has identical abnormal P waves (non-sinus P waves), which distinguishes it from ST. They may be inverted, but because they precede each QRS with a normal PR interval, it can be distinguished from a junctional tachycardia.
- Atrial flutter (A flutter) is a specific type of AT.Look for distinct fibrillation (F) waves in a sawtooth pattern. The atrial rate is 200-400 bpm, depending on the conduction ratio, and typically has a pattern associated with it (unlike A Fib). The rhythm is dependent upon the degree of AV block – a 2:1 block will have two flutter waves for each QRS, resulting in a fast ventricular rate (~150 bpm). A 3:1 and 4:1 block will have 3 and 4 F waves per QRS respectively, with ventricular rates of ~100 and ~75, respectively.
- Atrial fibrillation (A Fib). The atrial rate is typically 400-600 bpm, and has no distinct P wave morphology. The atrial activity may be coarse, fine, or non-existent. The ventricular rhythm is irregularly irregular and when the rate is >100 bpm, it is denoted as A Fib with rapid ventricular response (RVR). However, when F waves are >0.5 mm, it can be confused with A flutter (see our above paragraph on this).
- Multifocal atrial tachycardia (MAT). Again, this is often confused with A fib because the ventricular rhythm is irregularly irregular. MAT is similar to AT, but with at least three different P wave morphologies and varying PR intervals.
- Junctional tachycardia (JT). It typically begins as an accelerated junctional rhythm, with the heart rate gradually increasing until it surpasses 100 bpm. Most of the time (but not always), the retrograde P waves are typically, but not always, inverted in II, III and aVF, and may come before, during, or after the QRS complex. Remember that the P waves are retrograde – junctional rhythms are happening because a focus in the AV node is the primary pacemaker. PR interval is <120 ms, again, because the AV node has taken over. Types of JT:
- AVNRT (mentioned above in SVT)
- AV Re-entrant tachycardia. This rhythm occurs with the Wolff-Parkinson-White syndrome. It may be orthodromic or antidromic.
- Permanent form of junctional reciprocating tachycardia (PFJRT or PJRT).
- Junctional ectopic tachycardia (JET). Very rare, congenital tachycardia with a high mortality rate in infants.
- Supraventricular tachycardia (SVT or PSVT). This term is often used as a “catch all” for most ectopic tachy rhythms originating in the atrium, however, it does have it’s own distinctions. PSVT typically starts and stops abruptly and is >135 bpm. QRS is typically narrow.
- Ventricular tachycardias (VT). VT can be mono- or polymorphic (have one or multiple foci), and can be non-sustained or sustained. A broad QRS, extreme deviation from normal axis, and AV dissociation are three features of VT.
- If it is <30 seconds, it is non-sustained VT. Greater than 30, then it is sustained.
- Monomorphic VT. A singular focus with a regular rhythm. The QRS morphology is uniform.
- Idiopathic VTs: Right or Left Outflow Tract VT (ROVT or LOVT). These are typically not life-threatening and unrelated to structural heart disease.
- Fascicular tachycardia (idiopathic fascicular tachycardia).
- Polymorphic VT (PMVT). Multiple foci contribute to the QRS variations seen in this dysrhythmia, which also causes an irregular rhythm. The amplitude and width of each QRS are not identical.
- Torsades de Pointes (TdP). A specific type of polymorphic VT that appears due to QT prolongation. The bizarre, wide QRS seems to pulse in amplitude, “twisting” around a singular, imaginative point. It may be paroxysmal and not sustain for > 30 seconds.
- Bidirectional VT. The QRS axis alternates 180 degrees every other beat, and therefore appears positive and negative in relevance to the isoelectric line. This rhythm is very rare.
- Ventricular flutter (V flutter). This VT has no identifiable P or T waves. There are no aspects of the QRS that can be easily identified, and the amplitude is typically extreme. It could be easily confused with TdP.
- Ventricular fibrillation (V Fib). The amplitude may be course or fine, and the ECG strip looks like the heart is quivering. There is no definition in any wave morphology. The ventricular rate may typically approach ~500 bpm. It is often preceded by R-on-T PVC’s or VT. (Video of a heart in V Fib).
Dysrhythmia or arrhythmia?
This may be trivial, but I found it interesting. According to Dr. Kenneth D. Kronhaus, who published an abstract to the editor of the Journal of the American Medical Association (JAMA) in 1973, the proper term is dysrhythmia. Arrhythmia means “without rhythm,” so it technically cannot be used as a blanket term, even though most of the time it is. According to Kronhaus, “The term ‘dysrhythmia’ is not limited to irregularities of the heartbeat, but also is applied to disturbances of rate and conduction.”
Pacemakers: When they don’t work.
Tricky tricky… especially if you work at a specialized cardiovascular clinic or hospital. First, here is a link to some basics about how pacemakers work, and how normal ECG rhythms look with various types of pacemaker setups (i.e. atrial only, dual AV, whether or not sensing in triggered or inhibited, etc.)
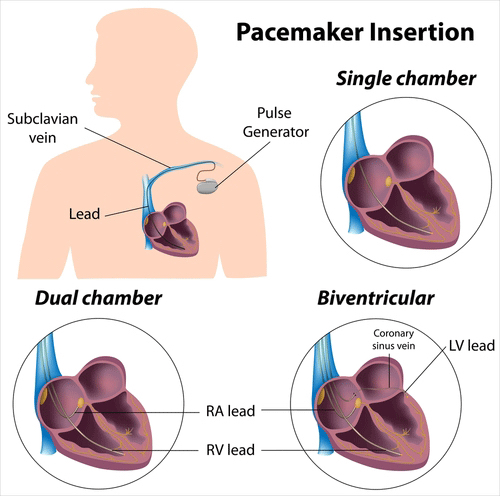
Now, here are a few common issues that happen with pacemaker malfunction, with simplified explanation:
Failure to fire/failure to pace. The device does not send an impulse where it is expected. On an ECG, a pacer spikes are missing.
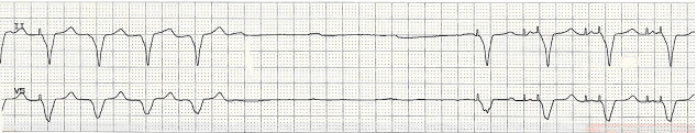
Failure to capture. The pacer fires, but myocardial depolarization does not result. On an ECG, pacer spikes are present, but there is no electrical activity (contraction) following.
Undersensing/Failure to sense. If spikes appear where they shouldn’t, such as within or after a QRS complex, then undersensing could be the problem. Undersensing happens when the pacemaker fails to detect the natural underlying rhythm.
Oversensing. Basically, the opposite of undersensing. The pacemaker thinks it senses natural electrical activity that is from a different source or doesn’t exist, and therefore is not activated. The pacemaker could be too sensitive.
For more on malfunctions, such as runaway pacemaker and pacemaker-mediated tachycardia (PMT), click here.
And finally, a really cool link: A battery-less pacemaker that regenerates its energy from the heart’s own electricity.
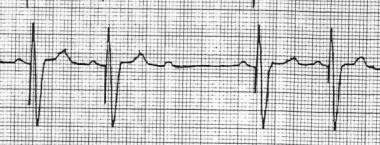
Can junctional rhythms have a positive P wave in lead II?
Yes, but not often, and it depends on the anatomical location of the ectopic focus. Let’s start old, as the old research set the foundation on how we practice today. In 1973, Dr. Kenneth M. Rosen published an article in Circulation on junctional tachycardia. He dove into wave morphology, and referenced several previous studies on P wave morphology. Several had concluded that rhythms which produce upright P waves in leads II, III and aVF arise from an origin near the carotid sinus.
Another article published in Circulation circa 1973, this time by Dr. Benjamin Scherlag et al., analyzed the rhythms associated with the five pacemaker sites (at the time) located within the AV junction. The ECG tracing associated with a focus located at the His bundle shows a positive P wave morphology:
Fast forward. The British Medical Journal (BMJ) published an article in 2002 entitled, “ABC of Clinical Electrocardiography: Junctional Tachycardias.” Here, only two types of JT were covered, AVNRT and AV re-entrant tachycardia. AVNRT has inverted P waves if before the QRS, but are more often buried or after the QRS due to the re-entry circuit. Orthodromic AV re-entrant tachycardia, as a part of Wolff-Parkinson-White syndrome, will show delta waves as an augment to the R wave until the tachy sets in, which is not to be confused with a positive P wave in leads II and III. At the point where the tachycardia is present, no delta waves are seen, and P waves follow the QRS complex.
In 2015, Dr. Carmelo Buttà and colleagues at the Biomedical Department of Internal and Specialist Medicine, University of Palermo, Italy, did a thorough research review of atrial tachycardias. The article, published in the Annals of of Noninvasive Electrocardiology, reviewed several current electrocardiographical findings regarding ectopic atrial tachycardias, including JT and PFJRT (permanent form of junctional reciprocating tachycardia). Buttà stated that “JT may rarely present retrograde P waves before QRS complex (negative on the inferior leads and positive in V1),” the inferior leads being II, III and aVF. This is dependent on the location of the focus, again, and a focus located near the carotid sinus may show positive P wave morphology in a junctional tachycardia.
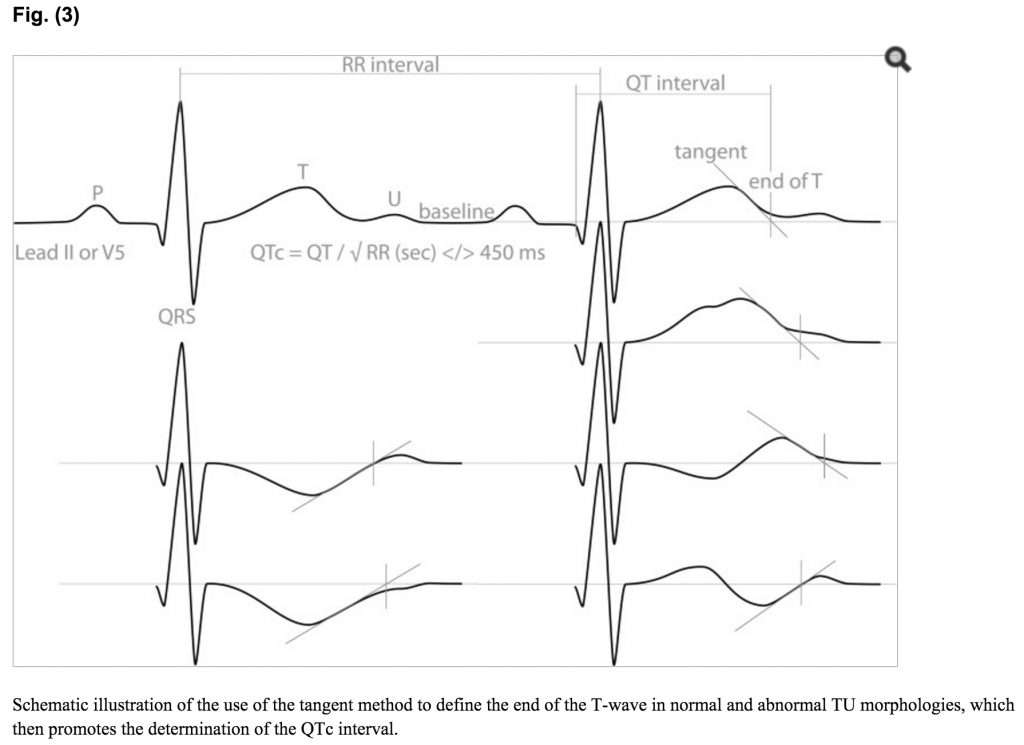
Measuring the QT Interval
Sometimes, it is difficult to find where the T wave ends, making an accurate measurement of the QT inveral difficult. Variability in T wave morphology is high, with individuals having biphasic, inverted and peaked T waves, to name a few. Then add in ST segment elevation and depression, and accurate measurement on an ECG strip may become even harder. I’m sure I see a wider array of morphologies working at a specialized heart hospital, however, that does not make this any less important.
I found an excellent article published by Dr.’s Pieter G Postema and Arthur A.M Wilde in 2014, entitled The Measurement of the QT Interval. By the obvious title alone, it was definitely worth checking out. They do a nice job discussing the history, physiology and math regarding the measurement of the QT interval, going into depth re: U waves, correction factors, disrhythmias and length, and end with some tips and tricks. Here is a link to the full article on PubMed – it is definitely worth your time.
I did want to pull out one figure in particular, as it gives a good visual of some commonly encountered T wave morphologies, and how to go about finding the end of the wave using the tangental method.
References:
Badhwar, N., & Scheinman, M. M. (2007). Idiopathic ventricular tachycardia: diagnosis and management. Current problems in cardiology, 32(1), 7-43.
Buttà, C., Tuttolomondo, A., Giarrusso, L., & Pinto, A. (2015). Electrocardiographic Diagnosis of Atrial Tachycardia: Classification, P‐Wave Morphology, and Differential Diagnosis with Other Supraventricular Tachycardias. Annals of Noninvasive Electrocardiology, 20(4), 314-327.
Esberger, D., Jones, S., & Morris, F. (2002). ABC of clinical electrocardiography: junctional tachycardias. BMJ, 324(7338), 662.
Hoppe, B. L., Kahn, A. M., Feld, G. K., Hassankhani, A., & Narayan, S. M. (2005). Separating atrial flutter from atrial fibrillation with apparent electrocardiographic organization using dominant and narrow F-wave spectra. JACC, 46(11), 2079-2087.
Hujier, Fares. (Telemetry Monitor Technician and Cardiologist). Personal interview and EKG monitor technician orientation (2016).
Leal, M. Principles of Cardiac Pacing. University of Wisconsin. Retrieved on Jun 27, 2016 from http://www.uwhealth.org/files/uwhealth/docs/pdf6/eec_courses/paramedic_training_60/principles_of_cardiac_pacing.pdf
Postema, P. G., & Wilde, A. A. M. (2014). The measurement of the QT interval. Current cardiology reviews, 10(3), 287-294.
Prystowsky, E. N., Padanilam, B. J., Joshi, S., & Fogel, R. I. (2012). Ventricular arrhythmias in the absence of structural heart disease. Journal of the American College of Cardiology, 59(20), 1733-1744.
Rosen, K. M. (1973). Junctional tachycardia Mechanisms, diagnosis, differential diagnosis, and management. Circulation, 47(3), 654-664.
Waktare, J. E. P. (2002). Cardiology patient page: Atrial fibrillation. Circulation. 106: 14-16. doi: 10.1161/01.CIR.0000022730.66617.D9. Retrieved from http://circ.ahajournals.org/content/106/1/14.full
Pingback: Cardiovascular Adaptations to Exercise and the Athlete EKG • truPhys