Pain is one of the most difficult conditions to diagnose, a seemingly invisible disability. It is relative to the individual mind and body, manifests at different amplitudes, and often relies on good communication and understanding between the practitioner and patient to successfully determine its etiology. There is no cure for most chronic pain syndromes, and unfortunately, cannabidiol (CBD) isn’t one either. However, CBD is proving its usefulness in several areas of medicine, and the growing body of evidence is warranting a further look into the comparative effectiveness of it as a drug used in pain management.
What is chronic pain syndrome?
Chronic pain typically stems from an acute illness or injury and is defined by pain that persists longer than six months. If the chronic condition is accompanied by secondary complications that cause an increased amount of pain or heightened sensitivity to pain, it is considered a chronic pain syndrome. Complications include mood disturbances like depression, anger and anxiety. Often, patients that suffer from chronic pain syndrome experience a decrease in their quality of life.
There isn’t a one-size-fits-all reason that someone may experience chronic pain. It may manifest from a rheumatic disorder, while others are neuropathic in nature. For some, pain may be localized, such as in the lower back, and others may experience pain throughout their body. Patients may also experience hyperalgesia, an increased sensitivity to painful stimuli resulting from neural damage. It may also be induced by opioid use. For a more comprehensive list of conditions, visit the American Chronic Pain Association website.
Migraines, irritable bowel syndrome (IBS), rheumatoid and osteoarthritis are a few familiar conditions that can lead to chronic pain syndrome. Fibromyalgia is characterized by chronic musculoskeletal pain, mood disturbances including depression, and fatigue. Multiple sclerosis (MS) presents its own symptomology and can be highly varied between individuals, but similar to fibromyalgia, includes pain, fatigue, and depression, and additionally, muscle spasticity and inflammation. Neuropathic pain may present as a complication from diabetes. Other types of chronic pain can manifest from previous injury and soft tissue damage, and also from cancer.
Why CBD for chronic pain syndrome?
There is a growing body of supportive evidence associating the various mechanisms behind CBD’s therapeutic actions and the treatment of conditions that cause chronic pain and lead to chronic pain syndrome. Right now, it is not approved by the FDA to treat chronic pain, but research is underway (more on this later). Currently, there are several classes of drugs prescribed to treat chronic pain. Here is a list of examples:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Naproxen, ibuprofen
- COX-2 inhibitors
- Celecoxib (Celebrex)
- Analgesics and Opioids
- Acetaminophen
- Hydrocodone, hydrocodone-acetaminophen, fentanyl, oxycodone, oxycodone-acetaminophen
- Tricyclic anti-depressants
- amitriptyline and nortriptyline
- Serotonin-norepinephrine reuptake Inhibitors (SNRIs)
- duloxetine (Cymbalta), venlafaxine (Effexor XR) and milnacipran (Savella)
- Anti-epileptics
- Gabapentin, pregabalin (Lyrica)
There isn’t a set approach to pain management, especially taking into account the variety of causes that elicit pain. The current opioid crisis has shown the dangers of some of these drugs, and safer drugs aren’t necessarily without long-term side effects. In some cases, more than one treatment approach may be taken. Also, many treatments are combined with physical and occupational therapy, as well as cognitive behavioral therapy and other types of psychotherapy to teach patients how to better understand and emotionally regulate their pain, reducing its effects on everyday quality of life.
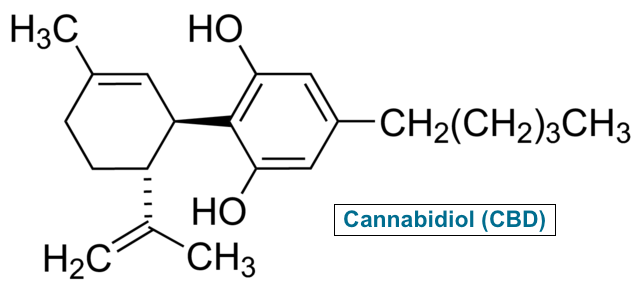
Where does CBD fit in? CBD acts as an anti-inflammatory drug, which may be beneficial for some types of arthritis and chronic pain stemming from injury and soft-tissue damage. Several studies have also investigated CBD’s mechanism as 5-HT1a receptor agonist. Similar to how some types of antidepressants work, CBD has shown to increase serotonin levels in certain areas of the brain. It also elicits effects on GABA receptors. (More in-depth information on CBD’s therapeutic mechanisms of action can be found here.)
It is difficult to prescribe CBD because its efficacy and effectiveness isn’t fully understood in relation to treating pain. But scientists are beginning to understand how it may be used in comparison to what we know already works. For example, duloxetine (Cymbalta), an SNRI antidepressant, is often prescribed to treat fibromyalgia. It affects a variety of sites throughout the body, and one particular site of action in the dorsal horn of the spinal cord. Basically, the drug increases the threshold of activation needed to send a pain signal to your brain. This is an important reason why it is used in fibromyalgia treatment, on top of the fact it also improves symptoms of depression associated with the disorder.
Researchers have found cannabinoid receptors in the same area of the spinal cord. Activation of these CB1 receptors has a similar and effective influence on pain. In addition, it is understood that “activation of peripheral CB2 receptors generates an antinociceptive response in situations of inflammatory and neuropathic pain,” (Manzanarez), essentially “blocking” the detection of a painful stimulus.
Studies also suggest that CBD may correct deficiencies in the body’s own endocannabinoid system (ECS). The ECS can be described as a “mothership” running in the background, dictating overall neurotransmitter balance, regulating pain, metabolism, sleep-wake, and even mood, focus and memory, and of course, pain. The ECS was only recently discovered in the 1990’s and research has been developing a theory that individuals suffering from certain chronic pain conditions may actually be suffering from an endocannabinoid deficiency. The theory was originally proposed in 2001.
Our body produces a variety of substances that interact with the endocannabinoid system, There have been suggestions that deficiencies in anandamide and 2-AG, both endocannabinoids, may be linked to chronic pain syndromes, and researchers are looking at whether or not certain cannabis compounds can be utilized to treat the deficiency, CBD being one of them. For more, check out this journal article published in 2016 by neurologist Dr. Ethan Russo.
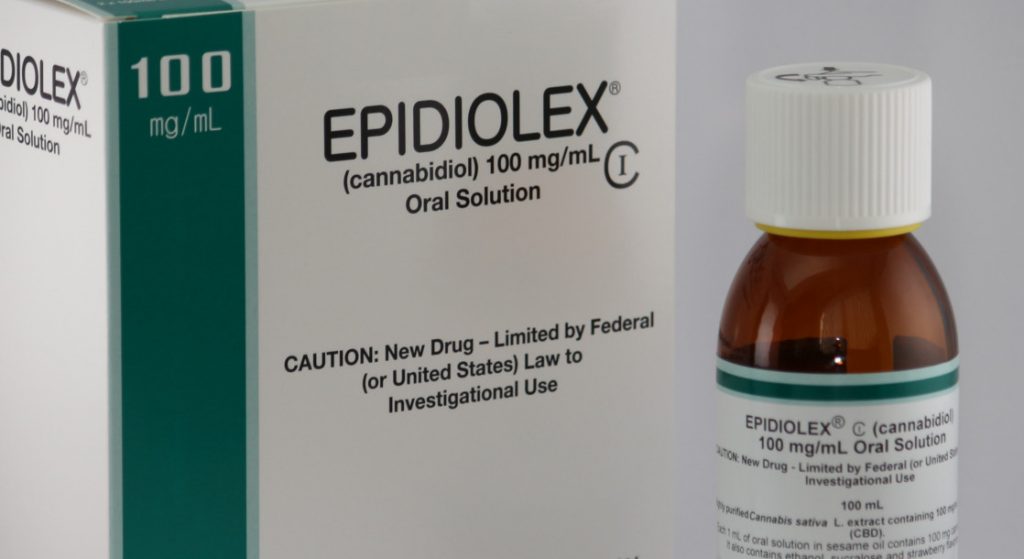
Researchers at Colorado State University are currently investigating whether or not CBD may be an effective treatment for improving impaired mobility, muscle spasticity, pain and fatigue in patients suffering from multiple sclerosis (MS), and results are promising. In addition, there are several well-designed clinical trials underway. Dr. Staci Gruber of Mclean Hospital, Harvard Medical School, is conducting Phase 2 of a double-blind, open-label randomized clinical trial investigating the efficacy of a sublingual CBD tincture for treatment of chronic pain. Another team at Massachusetts General Hospital in Boston is looking at the effects of CBD, specifically, Epidiolex, on low back pain stemming from neuroinflammation. For a list of all clinical trials registered with the National Library of Medicine, click here.
The symptomatic relief provided by CBD may result from a combination of decreased soft tissue inflammation as well as an augmentation of mood and the processing of pain, suggesting it may be a beneficial alternative for some patients who are seeking a more natural alternative to other medications, who may have limitations to certain drugs, or are looking for something with less adverse effects, though more research needs to be conducted.
How do I use CBD to treat chronic pain?
Patients interested in trying out CBD derived from hemp and/or any products also containing a small amount of THC should consult their physician to see if it is a right fit for their treatment regimen. There are several options patients may consider depending on their experience using CBD or other cannabis formulations.
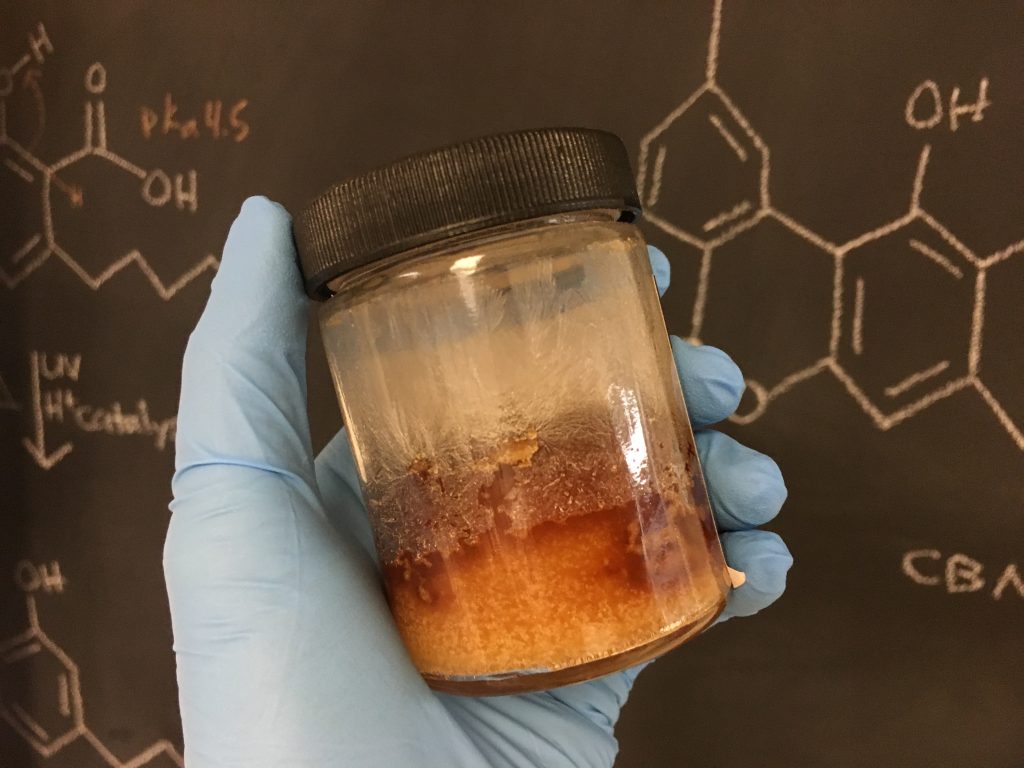
It is important to choose a manufacturer that can provide a certificate of analysis ensuring any label claims are true. This information includes dosing and concentration of CBD, as well as solvents used in the production process. In addition, choosing a full-spectrum product that contains other compounds from the plant is supported to be more beneficial than isolated CBD on its own. Last, look for a product made from hemp that is grown without pesticides and other harmful chemicals.
Patients are recommended to “start low and go slow.” Microdosing is a great way to help ensure a therapeutic dose is administered with a very minimal risk of experiencing side effects. It’s suggested patients with little to no experience consuming CBD begin with 10-15 mg of CBD per dose in a full-spectrum formulation. If positive effects are not experienced, an increase in dose is warranted. The dose will be dependent on ECS tone, tolerance, and severity of pain, so a dose upwards of 50 mg may be necessary – again, it all depends.

Research does support choosing a product containing a small amount of THC for improved pain management. By microdosing, the intoxicating (“high”) properties associated with THC becomes minimal or non-existant. Again, it is all up to the patient to determine what is right for them so they can confidently manage their pain.
References:
Atzeni, F., Talotta, R., Masala, I. F., Giacomelli, C., Conversano, C., Nucera, V., … & Bazzichi, L. (2019). One year in review 2019: fibromyalgia. Clin Exp Rheumatol, 37(Suppl 116), 3-10.
Booz, G. W. (2011). Cannabidiol as an emergent therapeutic strategy for lessening the impact of inflammation on oxidative stress. Free Radical Biology and Medicine, 51(5), 1054-1061.
Corso, J. L. (2018, August 8). The Mind-Body Connection to IBS • truPhys. Retrieved February 14, 2020, from https://truphys.com/ibs-irritable-bowel-syndrome/
Corso, J. L. (2019, March 20). What Is the Therapeutic Value of CBD? • truPhys. Retrieved February 14, 2020, from https://truphys.com/the-therapeutic-value-of-cbd/
Habib, G., & Avisar, I. (2018). The Consumption of Cannabis by Fibromyalgia Patients in Israel. Pain research and treatment, 2018, 7829427. https://doi.org/10.1155/2018/7829427
Habib, G., & Artul, S. (2018). Medical cannabis for the treatment of fibromyalgia. JCR: Journal of Clinical Rheumatology, 24(5), 255-258.
Helpful for chronic pain in addition to depression. (2019, October 5). Retrieved February 14, 2020, from https://www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/art-20044970
Manzanares, J., Julian, M., & Carrascosa, A. (2006). Role of the cannabinoid system in pain control and therapeutic implications for the management of acute and chronic pain episodes. Current neuropharmacology, 4(3), 239–257. https://doi.org/10.2174/157015906778019527
Rudroff, T., & Sosnoff, J. (2018). Cannabidiol to Improve Mobility in People with Multiple Sclerosis. Frontiers in neurology, 9, 183. https://doi.org/10.3389/fneur.2018.00183
Russo, E. B. (2016). Clinical endocannabinoid deficiency reconsidered: current research supports the theory in migraine, fibromyalgia, irritable bowel, and other treatment-resistant syndromes. Cannabis and cannabinoid research, 1(1), 154-165.
White, C. M. (2019). A review of human studies assessing cannabidiol’s (CBD) therapeutic actions and potential. The Journal of Clinical Pharmacology, 59(7), 923-934.
Very informative. Answered many questions I had regarding CBD and it’s benefits.
Thank you. I am very glad you found it resourceful!